| 哺乳动物的妊娠起始于囊胚的滋养层细胞与子宫内膜识别、黏附,并进一步向子宫内膜侵袭,将胚胎锚定在子宫壁上。伴随胚胎发育,胚胎滋养层细胞活跃增殖和分化,对子宫内膜基质和螺旋动脉进行改建和重构,建立完善的子宫-胎盘-胎儿循环,保障胎儿宫内发育。因而,胎盘发育是哺乳动物妊娠成功建立和维持的重要保障。胎盘发育不完善将引起一系列复杂的妊娠相关疾病,如子痫前期、复发流产、胎儿生长受限等,对母儿近远期健康都造成严重危害。 迄今,对人类胎盘的认识依然是个“黑匣子”,其发育调控机理及其介导的母体妊娠适应性调节机制仍有待阐明,而与之密切相关的妊娠重大疾病的预测、防治和干预也亟待突破。 本研究组在前沿科学问题和国家重大需求引导下,致力于研究胎盘发育和妊娠维持的调控机制,以及妊娠高血压、复发流产等重大妊娠疾病的发病机理。旨在揭开人类妊娠健康的神秘面纱,并为发展重要妊娠疾病的预测和干预策略奠定坚实的科学基础。 揭示了人类滋养层干细胞命运决定和功能特征的代谢及表观调节机制,发现了mTOR-TFEB信号介导的滋养层细胞合体化通过巨胞饮方式适应环境营养压力的机制,阐释了蛋白质糖基化修饰调节滋养层细胞分化的路径;揭示了子宫螺旋动脉改建进程中血管内滋养层细胞的免疫调节功能及平滑肌细胞的去分化命运;系统阐释了母胎界面上妊娠适应性的细胞和分子调控网络,构建dNK细胞归巢到子宫的人源化小鼠模型并揭示了CD56brightCD39+ dNK细胞在妊娠维持中的重要作用机制;通过与多中心临床单位协作,建立了多种妊娠疾病前瞻性资源库,鉴定了子痫前期等妊娠疾病的早期预测标志物;解析了母胎界面多细胞互作及母体妊娠适应性的分子通路紊乱参与子痫前期、胎儿生长受限、复发性流产等疾病发生发展的机理。在Cell Stem Cell, Natl Sci Rev, PNAS等期刊发表研究论文百余篇。 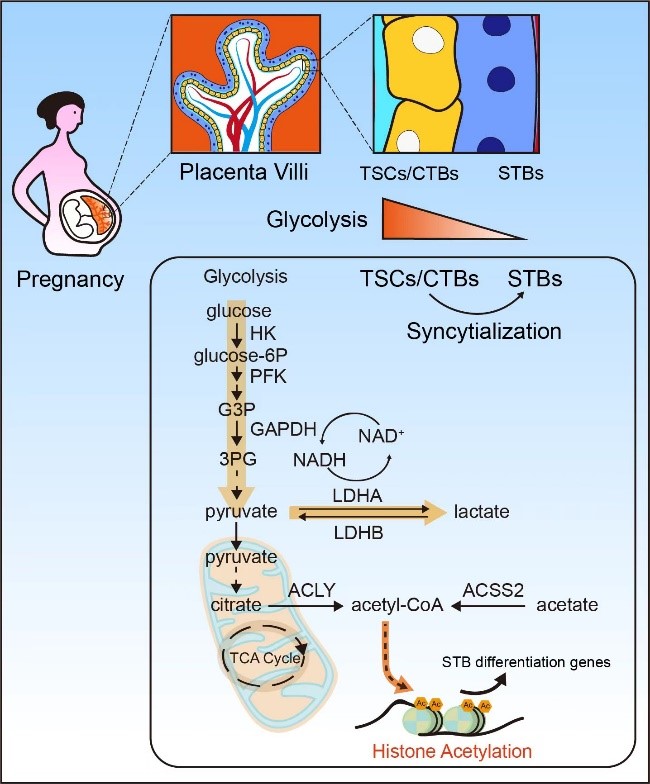
揭示人类滋养层干细胞命运决定和功能特征的代谢及表观调节机制(Cell Stem Cell 2024)
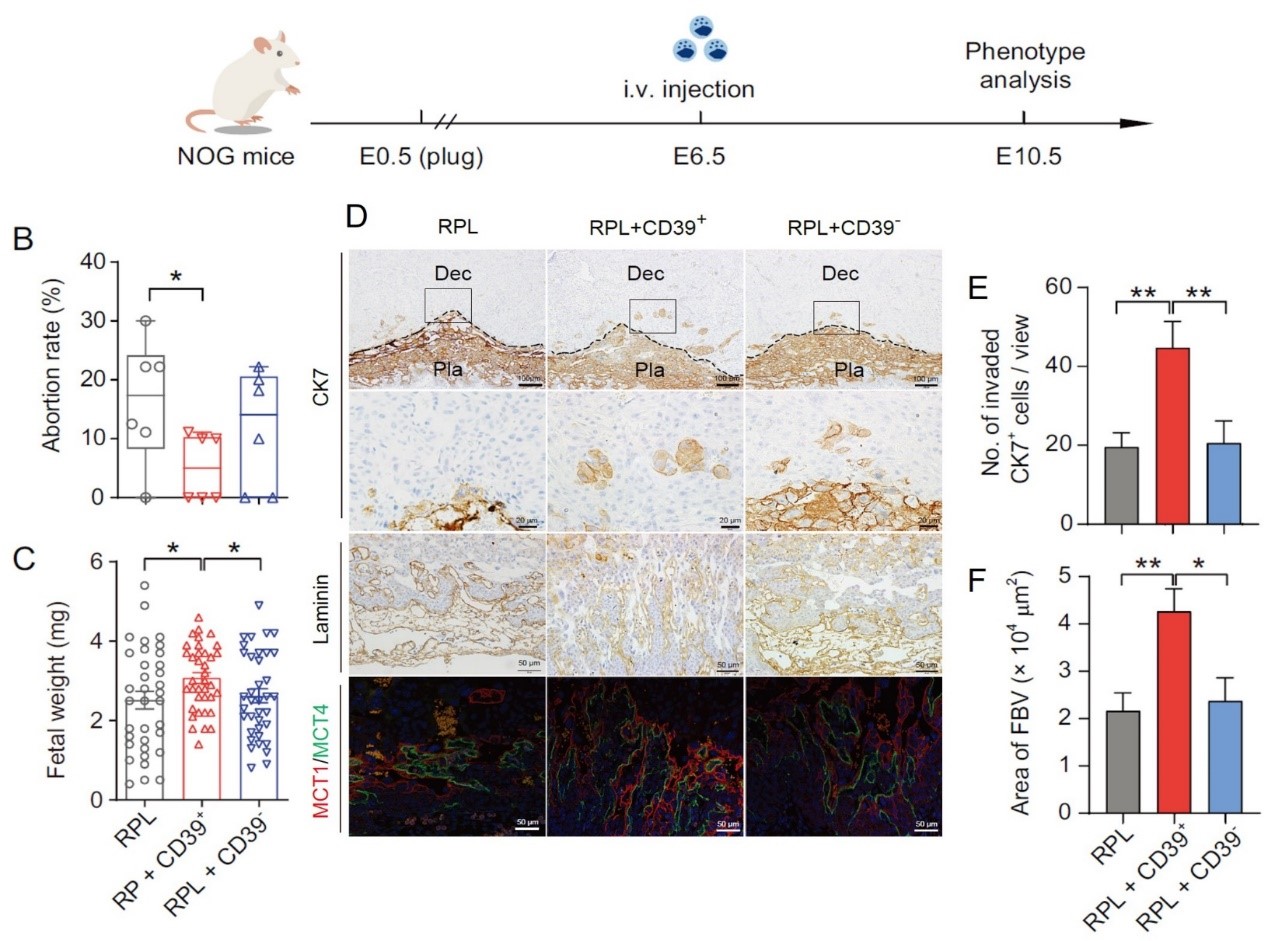
构建dNK细胞归巢到子宫的人源化小鼠模型并揭示CD56brightCD39+ dNK细胞在妊娠维持中的重要作用机制(Natl Sci Rev 2024)
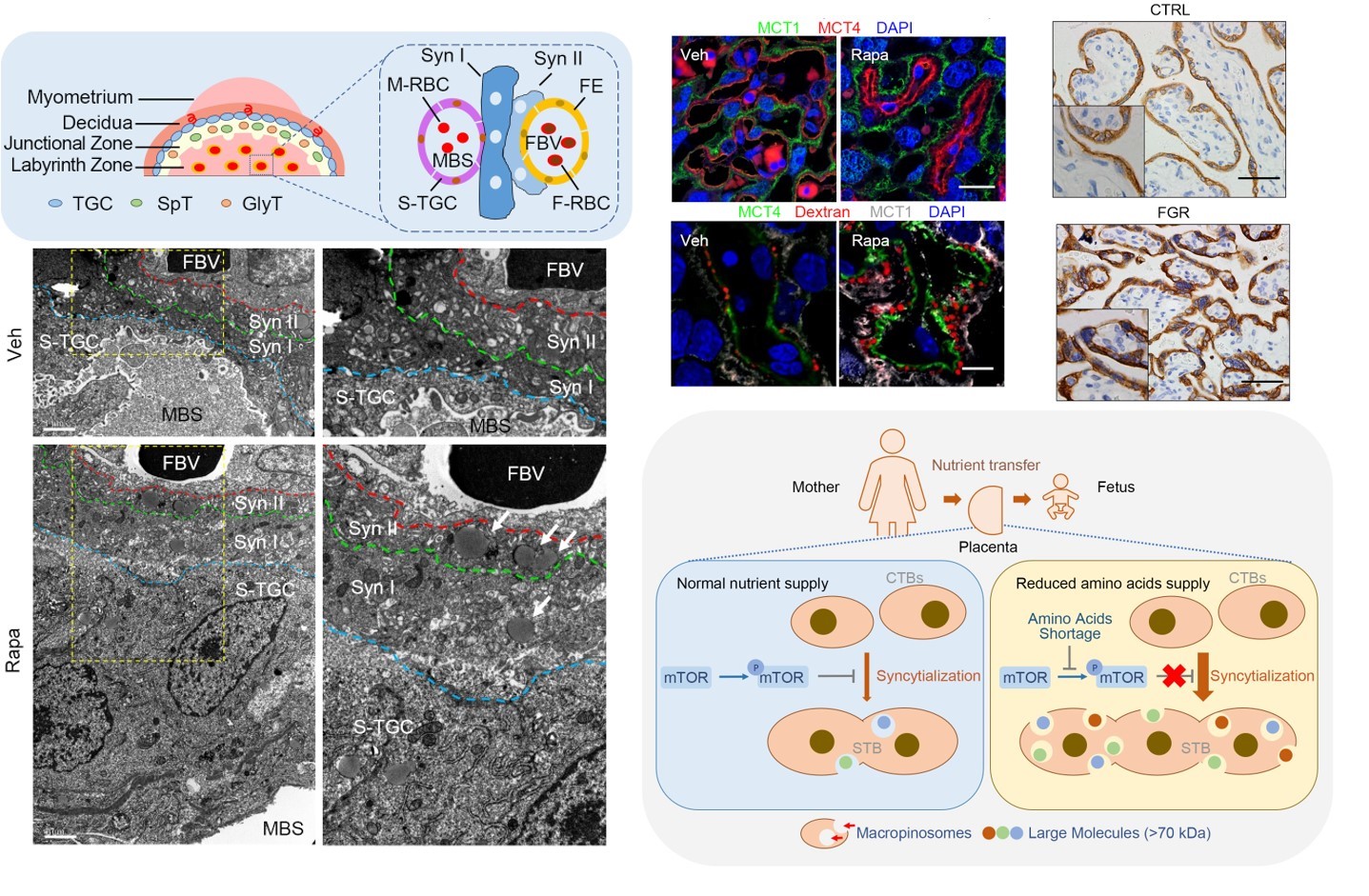
揭示了mTOR-TFEB信号介导的滋养层细胞合体化通过巨胞饮方式适应环境营养压力的机制(PNAS 2021, 2024)

揭示了子宫螺旋动脉改建进程中血管内滋养层细胞的免疫调节功能及平滑肌细胞的去分化命运(Biol Reprod 2021, Cell Prolif 2020)
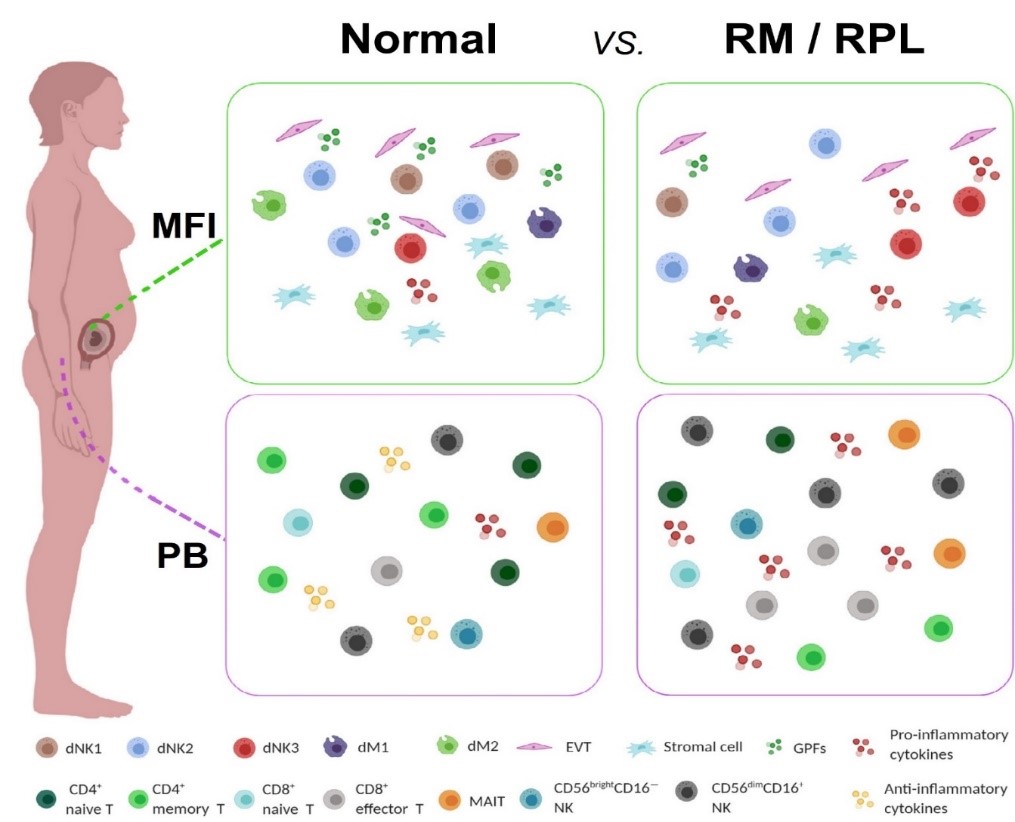
人类复发性流产的单细胞免疫景观(Genomics Proteomics Bioinformatics 2021)
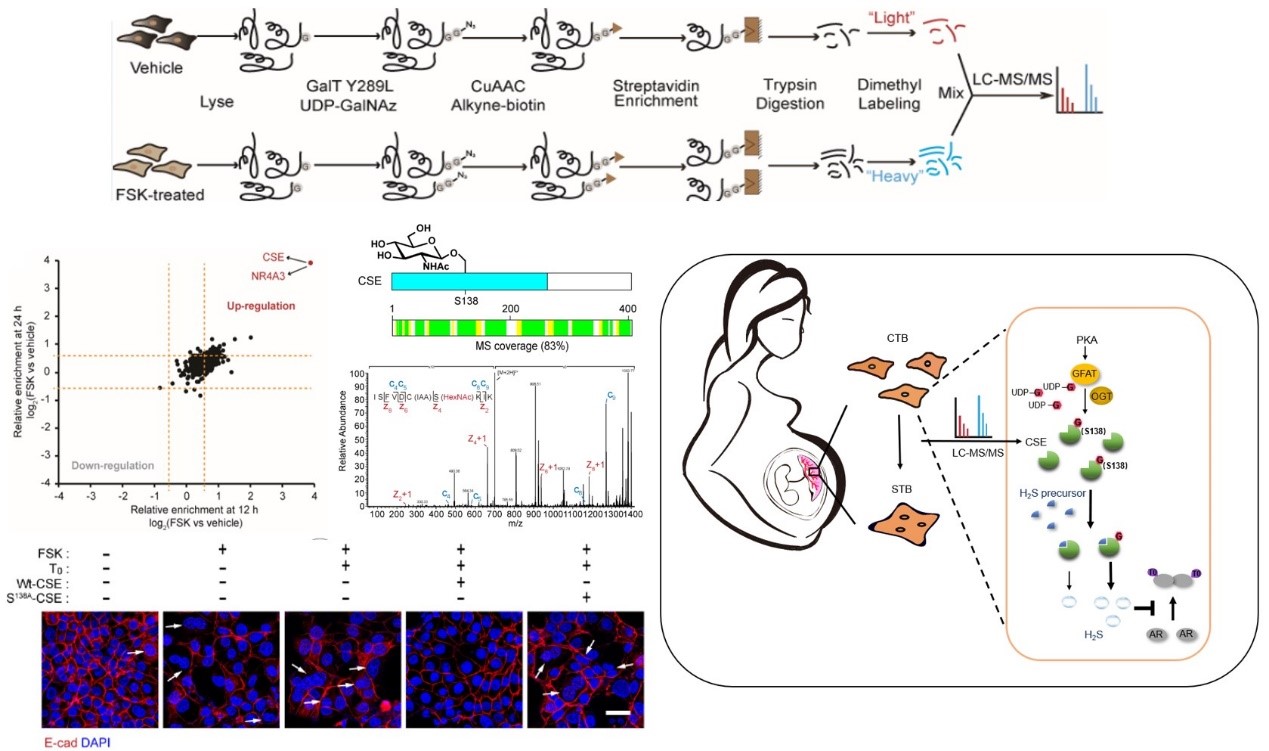
阐释了蛋白质糖基化修饰调节滋养层细胞分化的路径(Cell Chem Biol 2021)
| 研究内容和目标:
我们的主要研究兴趣是胎盘发育和妊娠维持的调控机制,并以此为切入点研究子痫前期和复发流产等重大妊娠疾病的病因学。具体的研究内容包括:
1. 胎盘滋养层细胞发育分化的谱系编程机制;
2. 子宫-胎盘-胎儿循环的构建机制;
3. 母胎界面多细胞互作建立免疫适应性的分子基础;
4. 子痫前期、复发流产等重要妊娠疾病的病因学。
研究目标是:综合利用临床样本库、体外模型和小鼠模型,将胎盘发育及功能研究与临床重大疾病机制和干预策略探索相结合,揭开人类胎盘发育和妊娠维持调控的分子机理,为发展重要妊娠疾病的预测和干预策略奠定坚实的科学基础。 代表性发表论文: - Yu X#, Wu H#, Su J#, Liu X, Liang K, Li Q, Yu R, Shao X, Wang H*, Wang YL*, Shyh-Chang N*. Acetyl-CoA metabolism maintains histone acetylation for syncytialization of human placental trophoblast stem cells. Cell Stem Cell. 2024 Sep 5;31(9):1280-1297.e7.
- Jia W#, Ma L#, Yu X#, Wang F, Yang Q, Wang X, Fan M, Gu Y, Meng R, Wang J, Li YX, Li R*, Shao X*, Wang YL*. Human CD56+CD39+ dNK cells support fetal survival through controlling trophoblastic cell fate: immune mechanisms of recurrent early pregnancy loss. Natl Sci Rev. 2024 Apr 11;11(6):nwae142.
- Zheng W#, Zhang Y#, Xu P, Wang Z, Shao X, Chen C, Cai H, Wang Y, Sun MA, Deng W, Liu F, Lu J, Zhang X, Chen D, Mysorekar IU, Wang H, Wang YL*, Hu X*, Cao B*. TFEB safeguards trophoblast syncytialization in humans and mice. Proc Natl Acad Sci U S A. 2024 Jul 9;121(28):e2404062121.
- Ma Y#, Yu X#, Ye S#, Li W, Yang Q, Li YX, Wang Y*, Wang YL*. Immune-regulatory properties of endovascular extravillous trophoblast cells in human placenta. Placenta. 2024 Jan;145:107-116.
- Li Y, Li Z, Wang C, Yang M, He Z, Wang F, Zhang Y, Li R, Gong Y, Wang B, Fan B, Wang C, Chen L, Li H, Shi P, Wang N, Wei Z, Wang YL, Jin L, Du P, Dong J, Jiao J. Spatiotemporal transcriptome atlas reveals the regional specification of the developing human brain. Cell. 2023 Dec;186(26):5892-5909.e22.
- Shao X#, Yang Y#, Liu Y#, Wang Y#, Zhao Y, Yu X, Liu J, Li YX, Wang YL*. Orchestrated feedback regulation between melatonin and sex hormones involving GPER1-PKA-CREB signaling in the placenta. J Pineal Res. 2023:e12913.
- Shao X#, Yu W#, Yang Y#, Wang F, Yu X, Wu H, Ma Y, Cao B*, Wang YL*. The mystery of the life tree: the placenta. Biol Reprod. 2022; 25;107(1):301-316.
- Li Y#, Li Z#, Yang M#, Wang F#, Zhang Y#, Li R#, Li Q, Gong Y, Wang B, Fan B, Wang C, Chen L, Li H, Ong J, Teng Z, Jin L*, Wang YL*, Du P*, Jiao J*. Decoding the temporal and regional specification of microglia in the developing human brain. Cell Stem Cell. 2022;29(4):620-634.e6.
- Chen J#, Du L#, Wang F#, Shao X#, Wang X, Yu W, Bi S, Chen D, Pan X, Zeng S, Huang L, Liang Y, Li Y, Chen R, Xue F, Li X, Wang S, Zhuang M, Liu M, Lin L, Yan H, He F, Yu L, Jiang Q, Xiong Z, Zhang L, Cao B*, Wang YL*, Chen D*. Cellular and molecular atlas of the placenta from a COVID-19 pregnant woman infected at mid-gestation highlights the defective impacts on fetal health. Cell Prolif. 2022;55(4):e13204.
- Li G#, Wang Y#, Cao G#, Ma Y, Li YX, Zhao Y*, Shao X*, Wang YL*. Hypoxic stress disrupts HGF/Met signaling in human trophoblasts: implications for the pathogenesis of preeclampsia. J Biomed Sci. 2022;29(1):8.
- Ma Y#, Yu X#, Zhang L#, Liu J, Shao X, Li YX, Wang YL*. Uterine decidual niche modulates the progressive dedifferentiation of spiral artery vascular smooth muscle cells during human pregnancy. Biol Reprod. 2021 Mar 11;104(3):624-637.(Editorial Choice; Faculty Opinions)
- Shao X#, Cao G#, Chen D#, Liu J, Yu B, Liu M, Li YX, Cao B*, Sadovsky Y*, Wang YL*. Placental trophoblast syncytialization potentiates macropinocytosis via mTOR signaling to adapt to reduced amino acid supply. Proc Natl Acad Sci U S A. 2021;118(3):e2017092118.
- Wang F#, Jia W#, Fan M#, Shao X#, Li Z, Liu Y, Ma Y, Li YX, Li R*, Tu Q*, Wang YL*. Single-cell immune landscape of human recurrent miscarriage. Genomics Proteomics Bioinformatics. 2021;S1672-0229(21)00003-6. (Editorial Highlight)
- Liu J#, Shao X#, Qin W#, Yanling Zhang#, Dang F, Yang Q, Yu X, Li YX, Chen X, Wang C*, Wang YL*. Quantitative chemoproteomics reveals O-GlcNAcylation of Cystathionine γ-lyase (CSE) represses trophoblast syncytialization. Cell Chem Biol. 2021;S2451-9456(21)00050-7. (Cover story)
- Ma Y#, Yang Q#, Fan M#, Zhang L, Gu Y, Jia W, Li Z, Wang F, Li YX, Wang J, Li R*, Shao X*, Wang YL*. Placental endovascular extravillous trophoblasts (enEVTs) educate maternal T-cell differentiation along the maternal-placental circulation. Cell Prolif. 2020;53(5):e12802.
- Shao X#, Wang Y#, Liu Y, Guo X, Li D, Huo R, Jia W, Cao G, Li YX, Liu M, Sha J, Zhao Y, Wang YL*. Association of imbalanced sex hormone production with excessive procoagulation factor SerpinF2 in preeclampsia. J Hypertens. 2019;37:197–205
- Shao X#, Liu Y#, Liu M, Wang Y, Yan L, Wang H, Ma L, Lia YX, Zhao Y*, Wang YL*. Testosterone represses estrogen signaling via upregulating mir-22: mechanism for imbalanced steroid hormone production in preeclampsia. Hypertension. 2017;69:721-730. (Editorial highlight)
- Xu P#, Zhao Y#, Liu M, Wang Y, Wang H, Li YX, Zhu X, Yao Y, Wang H, Qiao J, Ji L*, Wang YL*. Variations of micrornas in human placentas and plasma from preeclamptic pregnancy. Hypertension. 2014;63:1276-1284.
- Ji L#, Brkić J#, Liu M#, Fu G, Peng C*, Wang YL*. Placental trophoblast cell differentiation: physiological regulation and pathological relevance to preeclampsia. Mol Asp Med. 2013;34:981-1023.
|

